What Is Transitional Care and Why Is It Important?
Transitional care refers to the coordinated services that support patients as they move between healthcare settings. It’s essential because it:
- Reduces hospital readmissions
- Improves safety and continuity
- Enhances patient satisfaction
- Addresses both clinical and social needs
Continuity of care in transitional settings is essential for ensuring that patients receive comprehensive support during critical health transitions, minimizing gaps in treatment and enhancing overall outcomes. In today’s value-based environment, transitional care—when implemented with equity in mind—serves as a cornerstone for improved patient outcomes and more sustainable health care delivery. Learn more about our Transitional Care framework.
Understanding Social Determinants of Health
The World Health Organization defines SDOH as “the non-medical factors that influence health outcomes.” These include:
- Economic stability (e.g., income, employment, housing)
- Education access and quality
- Health care access and quality
- Neighborhood and built environment
- Social and community context
These elements shape health behaviors and influence whether individuals can adhere to discharge instructions, attend follow-up appointments, or manage chronic conditions such as congestive heart failure or cognitive impairment.
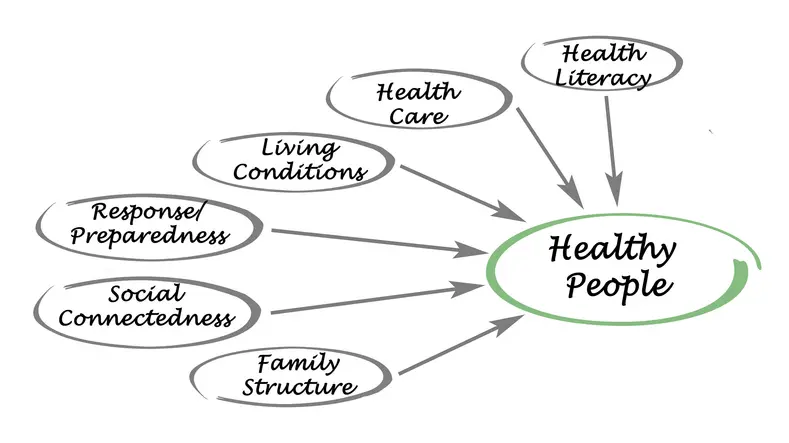
Social Determinants of Health and Transitional Care
Transitional care services (TCS) are designed to ensure continuity and coordination of healthcare as patients move between different care settings—such as from hospital to home or from acute care hospitals to rehabilitation services. While these services are clinically focused, their effectiveness is deeply influenced by factors that extend beyond traditional medical care. Social determinants of health (SDOH)—the conditions in which people are born, live, work, and age—play a critical role in the success or failure of transitional care across diverse health care settings. Since social risk factors like housing and food insecurity directly shape care outcomes, tracking transitional care effectiveness across SDOH helps reveal a fuller picture of success.
The Interplay Between SDOH and Transitional Care
Transitional Care and Healthcare Equity
Addressing Disparities in Access and Outcomes
Transitional care isn’t just a medical process—it’s a justice issue. Historically marginalized communities face deeper and more complex barriers during care transitions. Structural racism, language barriers, income inequality, and geographic isolation all increase the risk of poor outcomes. Transitional care plays a critical role in advancing health equity, particularly for historically marginalized patient populations. During periods of transition—such as after an episode of hospital care—individuals face elevated risks that are often compounded by structural disparities.
Populations impacted by racial, linguistic, or economic barriers often experience fragmented health care services, poor follow-up, and worsened health outcomes. These groups are more likely to lack access to quality health care providers or rehabilitation services.
Transitional care in these communities must include:
- Culturally and linguistically appropriate services (CLAS)
- Referrals for housing and transportation
- Health education tailored to appropriate literacy levels
- Integration with trusted health professionals and community-based organizations
- Screening and response tools for SDOH risks embedded in every care transition
Integrating Social Determinants of Health
Effective transitional care models recognize that treating the medical condition is not enough. Addressing SDOH—such as food insecurity, caregiver absence, or unsafe home environments—is essential to supporting vulnerable populations, especially Medicaid patients with chronic conditions. The value of transitional care is seen in our ECM services, read about our Enhanced Care Management and transitional services.
Multidisciplinary teams at the center of these models include:
- Social workers
- Peer support specialists
- Housing and legal resource navigators
These teams are supported by insights from randomized controlled trials, systematic reviews, and data from across the nation.
Policy and Program Alignment
Federal and state agencies are advancing equity-based models of care:
- CMS links payment incentives to reductions in disparities in hospital care
- California’s ECM and Community Supports target high-risk individuals with complex needs
- Medicaid 1115 waivers fund pilots for foster youth, unhoused populations, and justice-involved patients
Addressing social risk factors is only part of the equation; understanding the policy frameworks shaping transitional care management ensures programs are both equitable and compliant. These policy shifts aim to improve patient outcomes and reduce health care costs.
What Presidium Health Is Doing to Address SDOH and Advance Equity Through Transitional Care
At Presidium Health, we believe that advancing health equity begins with reimagining transitional care from the ground up. Our programs are designed not just to reduce readmissions but to bridge the systemic gaps that disproportionately affect vulnerable, high-risk patients.
Looking Ahead: Toward Equity-Centered Transitional Care
Transitional care has the power to improve lives- when done right. That means looking beyond discharge instructions and into the realities of people’s lives. Whether it’s helping an older adult safely recover at home or ensuring an individual has access to healthy food and follow-up care, addressing SDOH is what transforms good care into great outcomes. The transitional care landscape is shifting toward equity, context, and quality of life. Presidium Health’s Transitional Care is leading the transformation- one transition, one patient, and one community at a time.



