At Presidium Health, we believe that improving health outcomes starts with understanding what truly drives them. While clinical care is essential, it accounts for only a fraction of what shapes a person’s health. The real impact happens outside the exam room — in the everyday conditions people face at home, at work, in school, and in their communities.
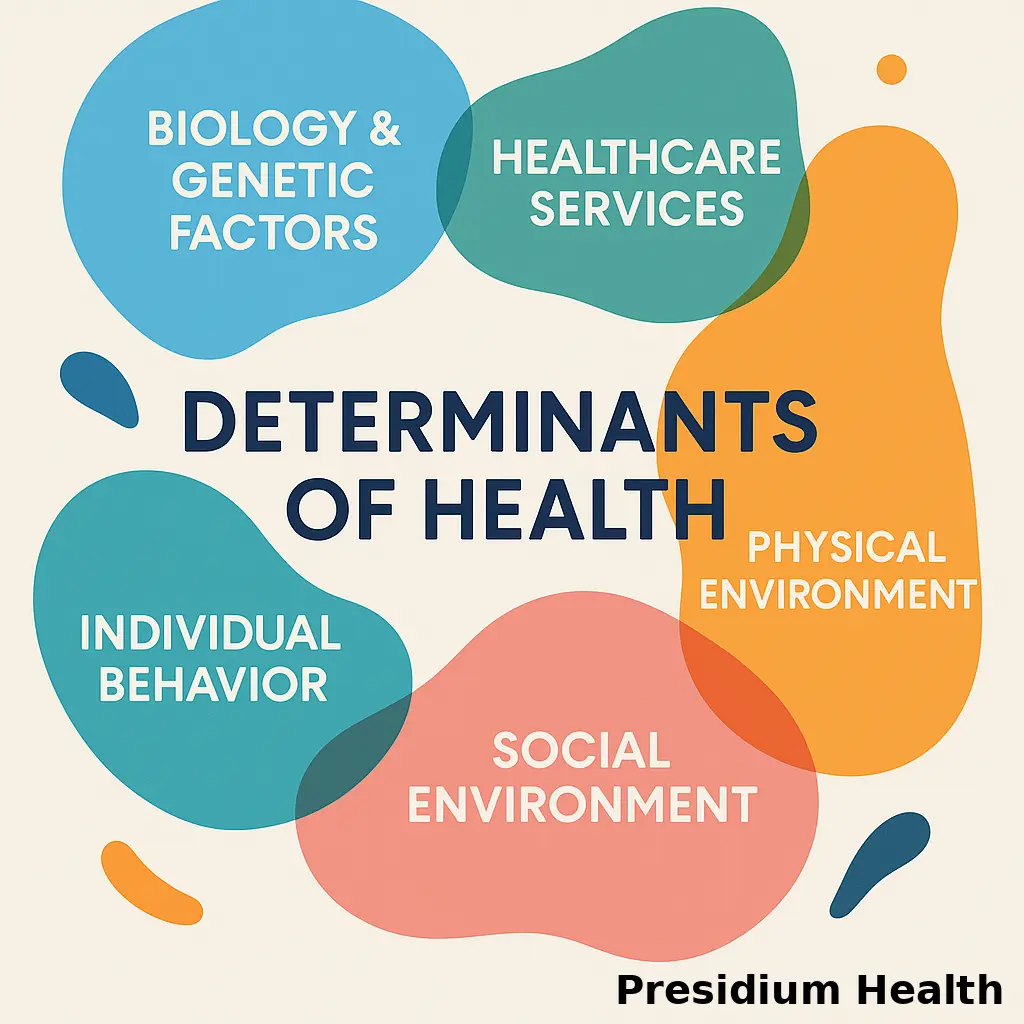
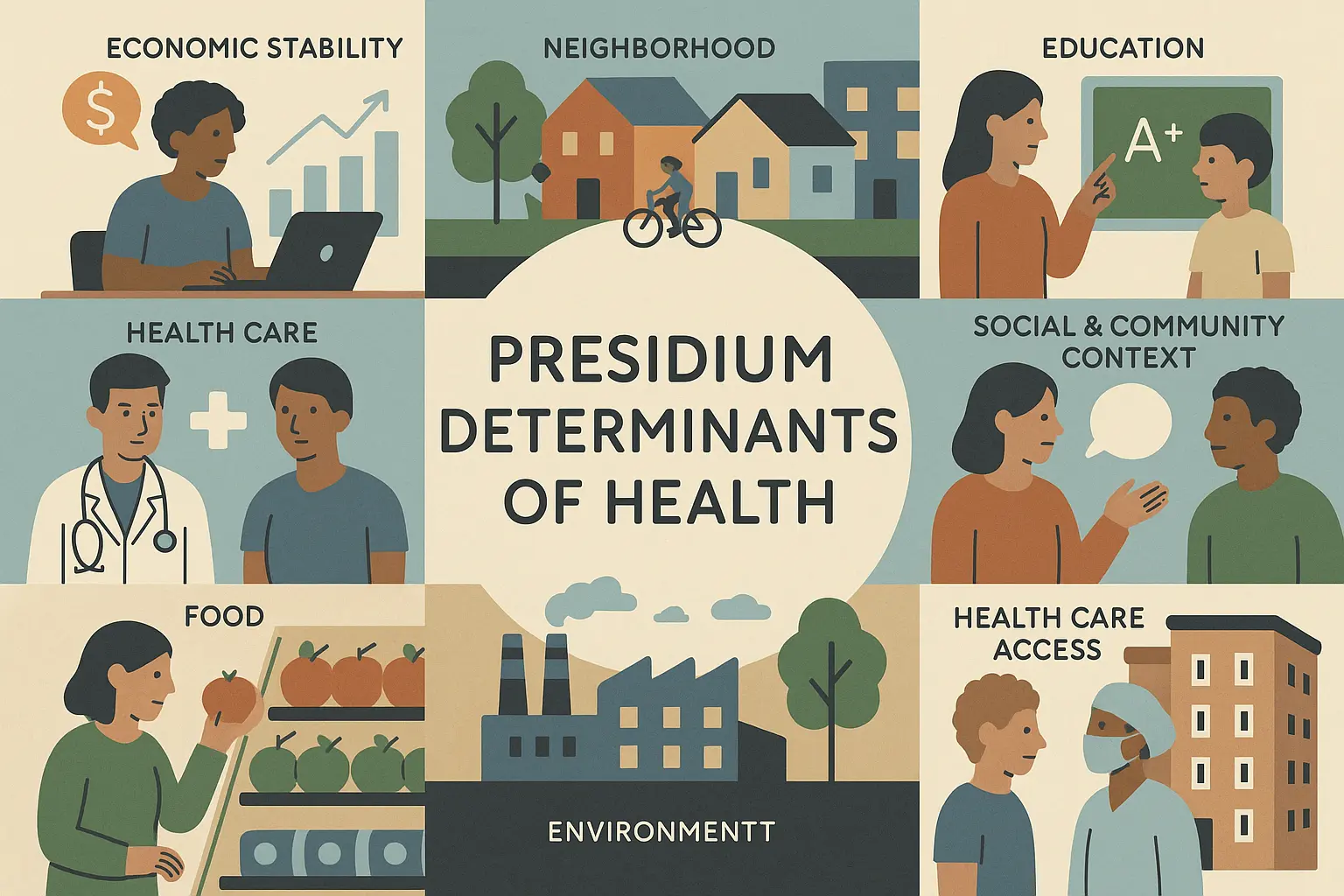
These conditions are known as Social Determinants of Health (SDOH) — the non-medical factors that influence physical and mental health outcomes are comprised of 5 domains. From access to nutritious food and stable housing to transportation, education, and social support, SDOH define the opportunities individuals have to live healthy lives.
The Approach: What Sets Presidium Health Apart
Explore how Presidium Health’s whole-person, equity-centered model compares to traditional providers. This comparison highlights our unique approach to social determinants of health (SDOH), Enhanced Care Management (ECM), and person-centered care delivery.
| Feature | Presidium Health’s Approach | Traditional Providers |
|---|---|---|
| Care Model | Wraparound, interdisciplinary | Fragmented by department or contract |
| Outreach | Proactive, in-home, flexible | Office-based, appointment-only |
| Cultural Competency | Trauma-informed, equity-driven | Standardized or generic |
| Integration | Social + medical + behavioral | Siloed services |
| Data + Tech | Real-time SDOH tracking integrated into workflows | Minimal or delayed SDOH tracking |
| Peer Engagement | Peer support is embedded and valued | Often absent or underutilized |
| Member Goals | Whole-person, self-defined | Utilization reduction focused |
| Alignment | CalAIM, Healthy People 2030, local CBO networks | Often disconnected from state/local context |
Understanding Social Health Determinants — And Why They Matter
Health begins long before a doctor’s visit—it starts at home, in schools, and within communities. Social Determinants of Health (SDOH) like housing, food, education, and transportation shape outcomes far more than prescriptions. You can’t treat chronic illness if someone can’t store their medication or get to their appointments. These unseen factors quietly drive disparities and costs across the system. Real care means addressing the root causes that live beyond the clinic walls.
Health Determinants vs Social Determinants: Understanding the Key Differences
Health is shaped by far more than medical care. From genetics and behavior to where we live, work, and grow, the determinants of health offer a comprehensive lens on what truly drives well-being. This article explores the interconnected factors that influence health outcomes—and why understanding them is essential for building more effective, equitable care systems
How Social Health Factors Impact Daily Life
Packed with gripping patient stories and eye-opening insights, this article brings Social Determinants of Health (SDOH) to life. It’s not theory. It’s the future of healthcare—and it’s already happening. Discover how interventions beyond medicine are rewriting the health script—and why ignoring SDOH is no longer an option.
California’s Social Health Landscape: Challenges, Trends, and Opportunities
California’s Social Determinants of Health (SDOH)—housing, food security, transportation, and education—are key drivers of health outcomes and inequities. It highlights Presidium Health’s equity-driven model, which integrates social needs directly into care through comprehensive assessments, multidisciplinary teams, and community partnerships. By addressing root causes alongside medical care, this approach aims to break down systemic barriers and create lasting health equity across California.
Social Health: How Connection Impacts Healthcare
Social health reflects the quality of relationships, belonging, and trust that support daily life. Strong social connections reduce isolation, strengthen resilience, and influence outcomes ranging from recovery after illness to long-term mental well-being. Explore how social health interacts with physical and mental health, why it is increasingly recognized as a public health priority, and how healthcare systems can restore connection through practical interventions.