The Hospital-at-Home model has expanded how acute care is delivered in the United States. By treating eligible patients in their own homes, this innovative approach eliminates the need for traditional hospital admissions, without compromising the quality of care. Dr. Pouya Afshar, CEO of Presidium Health, emphasizes, “This model is not just about convenience; it’s about delivering better outcomes and reducing hospital overutilization.” With 24/7 access to mobile clinicians, advanced monitoring technology, and personalized care, Hospital-at-Home has proven its effectiveness in reducing costs and improving patient satisfaction. To learn more about addressing care challenges, explore the Operation Care engagement platform.
Understanding the Hospital at Home Model
The Hospital-at-Home (HAH) model has emerged as a potentially transformative approach in health care delivery. By shifting care from traditional hospital settings to patient homes, it challenges conventional norms and prioritizes patient comfort, satisfaction, and healthcare cost of care reduction. As Dr. Afshar, CEO of Presidium Health, aptly noted, “This model is redefining acute care by making it more accessible and impactful for patients.”
Definition and Overview
Hospital-at-Home refers to a healthcare delivery model where eligible patients receive acute-level care in their homes instead of a hospital systems. Services typically include daily physician check-ins, remote patient monitoring, diagnostic testing, and 24/7 access to care teams. Clinical teams incorporated with home health, nursing, occupational and physical therapists ensures the patient receives the same holistic care they would receive in a hospital. This model is designed for patients with conditions like pneumonia, congestive heart failure, and certain infections that require hospital-level care but can be safely managed at home with advanced coordination.
Key features of the HAH framework include:
- Advanced Monitoring: Devices track vital signs and alert practitioners to any changes.
- Daily Provider Visits: On-site or virtual check-ups ensure continuity of care.
- Comprehensive Services: Health professionals extend beyond the clinical team. From medication management to physical therapy, it mirrors the hospital environment. Addressees healthcare needs and social determinants of health alike.
- Advanced Diagnostics: Easy access to radiology and lab services.
Dr. Afshar emphasizes, “This isn’t just an alternative; it’s an evolution of patient care, putting convenience and quality on equal footing.”
Benefits of Hospital at Home
The Hospital-at-Home model offers numerous advantages for patients and healthcare systems alike. Here’s why it’s gaining traction:
- Patient Comfort: Medical care in a familiar environment enhances peace of mind and speeds recovery. Ability to leverage family members in achieving safe care.
- Reduced Costs of Care: Studies show significant savings, with as much as 38% lower costs compared to traditional hospital stays. Learn more about cost-effective care solutions.
- Improved Outcomes: Reduced readmission rates and lower risks of hospital-acquired infections.
- Higher Patient Satisfaction: Patients appreciate the convenience and personalized attention of HAH programs.
- Decreased Hospital Strains: Improves health equity by freeing brick and mortar hospital beds for patients with more severe needs. Mitigate the importance of transitional care to improve readmission rates as patient does not suffer from change in venue.
As Dr. Afshar remarks, “The financial and personal impact of avoiding unnecessary brick and mortar hospitalizations is profound.”
Challenges and Considerations
Despite its potential, the Hospital-at-Home model isn’t without complexities. Healthcare providers and systems must consider these challenges:
- Eligibility: Not all patients qualify for HAH care. Eligibility depends on medical stability, home environment, caregiver support and most limiting, presentation to a brick and mortar emergency department.
- Emergency Preparedness: Robust protocols for sudden health deteriorations are critical in care of patients. Virtual triage and team deployment must be accessible and robust enough to function as an emergency department.
- Staffing Needs: Adequate training and availability of mobile care teams are essential for success.
These operational difficulties, as noted in a recent analysis, require a dedicated strategy to overcome.
Dr. Afshar adds, “Effective planning, clear protocols, and committed teams make all the difference. It’s about anticipating hurdles and staying one step ahead.”
By addressing these challenges, Hospital-at-Home programs can sustain their growth and usher in a new era of patient-centered care.
Distinguishing Between The Billable Service and The Service

In his paper –Hospital-At-Home: The Good, The Bad, The Ugly– Dr. Afshar distinguishes between hospital at home, the service line, distinct from the DRG billable service. He makes note of the inefficiency aligned with the DRG billable service requiring an ED visit. This in turn allows for an opportunity for a more efficient inpatient at home model that decouples the service line from the brick and mortar Emergency Room visit. Presidium Health has leveraged this efficiency in their value based model.
How Does the Cost of Hospital at Home Compare to Traditional Hospitalization?
Hospital at home services are typically more cost-effective than traditional hospitalization. Studies show that hospital at home programs can reduce costs by 30-70% compared to inpatient care, making it a financially efficient option for patients and healthcare providers alike.
The Role of Technology in Hospital at Home
Adopting the Hospital-at-Home model relies heavily on advanced technology to deliver care comparable to a traditional hospital environment. By integrating tools such as telehealth platforms and mobile healthcare teams, care providers ensure high standards of treatment within patient homes. Dr. Afshar, shares, “Technology bridges the gap between acute care needs and the comfort of being at home.”
Telehealth and Remote Monitoring
Telehealth and remote monitoring technology are the backbone of the Hospital-at-Home framework. These solutions allow healthcare teams to monitor patients in real time, ensuring safety and timely interventions.
- Telehealth Platforms: These enable virtual consultations, eliminating the need for frequent in-person visits. Patients can connect with physicians from the comfort of their homes, making care more efficient.
- Remote Patient Monitoring Devices: Devices like pulse oximeters and wireless ECG monitors track vital signs continuously. Alerts notify healthcare teams of abnormalities, enhancing response time.
Dr. Afshar highlights, “Remote monitoring allows us to act swiftly, minimizing risks while maximizing patient outcomes.” For professionals interested in understanding the technological drivers behind such programs, explore further here.
By leveraging these technologies, mobile healthcare teams can focus on clinical tasks while technical tools manage ongoing diagnostics. Read more on how innovative solutions address care disparities.
Mobile Healthcare Teams

Mobile healthcare teams serve as the physical extension of Hospital-at-Home programs. These trained professionals bring bedside care to the patient, replicating hospital-grade services without the walls.
- Multidisciplinary Teams: Mobile units often include physicians, nurse practitioners, and therapists. They coordinate seamlessly to deliver medications, administer treatments, and provide supportive care.
- Technology Integration: These teams use portable diagnostic devices and point-of-care tools to perform tests like bloodwork and imaging. Such versatility minimizes delays and bridges gaps in access.
Dr. Afshar aptly states, “With mobile teams, we’re taking the hospital to the patient, not the patient to the hospital.” Discover further insights into operational strategies in the Hospital-at-Home domain.
Technology and skilled healthcare teams work in unison, making Hospital-at-Home a feasible and efficient alternative to traditional care. This combination is transforming acute care delivery, showcasing a scalable model for future healthcare initiatives.
Presidium Health’s Value-Based Model

Presidium Health has reshaped at-home healthcare through its innovative value-based, incentive aligned care approach. With a focus on reducing costs and improving patient outcomes, the organization leverages advanced technologies and a patient-first ethos to redefine how healthcare is delivered to high-need populations. Presidium Health’s model has a focus on longitudinal care, across the acuity spectrum in a value-based care model.
Case Study Overview
Presidium Health’s pilot program in collaboration with San Diego’s Community Health Group offers a glimpse into the potential of value-based care. The program supported 93 medically complex patients, reducing hospitalizations by an impressive 53%. This success translated into a staggering $6 million in savings — an average of $65,000 per patient.
By emphasizing at-home, concierge-level care, Presidium tackled critical challenges in healthcare, addressing overutilization of expensive emergency rooms. As Dr. Afshar, explained, “Our mission is about achieving better results for those who need the most help. This is what quality-driven care looks like.” For a further information read how Presidium is expanding across California.
Quality Over Quantity
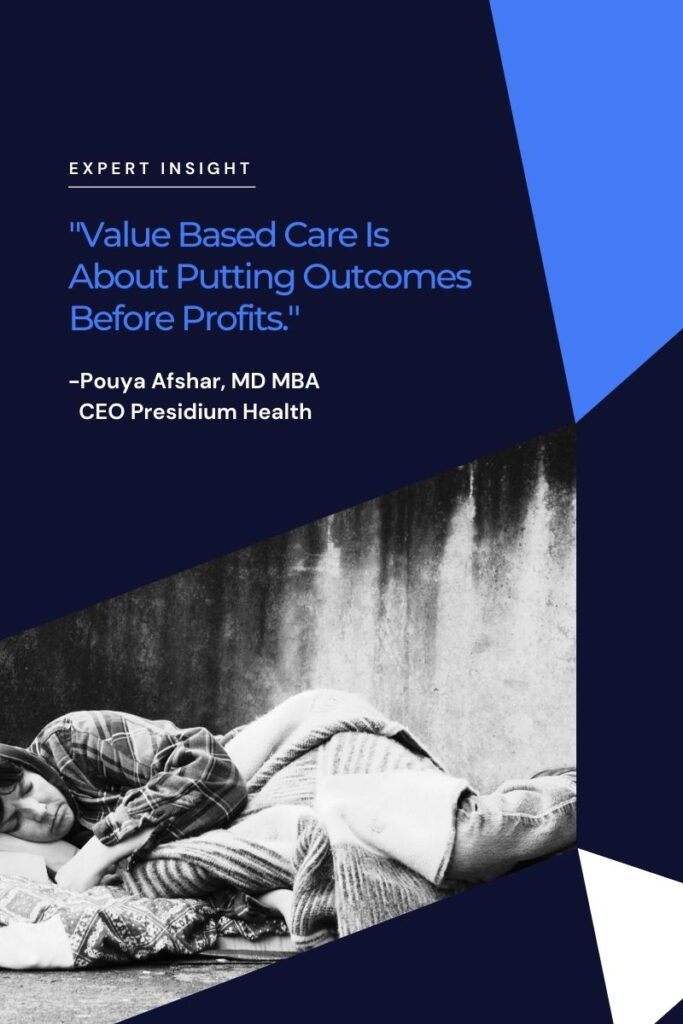
One of the defining principles of Presidium’s care model is prioritizing quality over quantity. This philosophy focuses on personalized, high-touch care, rather than serving the maximum number of patients. They have dubbed the moniker Concierge-Care-Without-The-Fare. Presidium notes their care model is excessive for many members, but is the answer for a population that has traditionally been neglected by the care system: underserved, hyper-utilizers.
During the pilot program, 24/7 access to medical providers and advanced primary care were accessible directly in patients’ homes. This eliminated the need for excessive hospital visits while ensuring their care met the highest standards. Dr. Afshar noted, “Value-based care is about putting outcomes before profits. It’s why we work to carefully design programs addressing individual needs, not just blanket solutions.”
Patients that required a step up in level of care were first evaluated by a virtual triage managed by a health care team accessible 24 hours a day 7 days a week. For appropriate conditions, if not able to resolve remotely, ancillary services and care teams would be deployed to the patient’s home. Management, discharge and transition back to routine care would then occur under one roof, with one team. Further step up in level of care could be accomplished through direct SNF admit or by leveraging the emergency room where appropriate.
This quality-focused approach didn’t just correlate with cost savings but also improved patient satisfaction and outcomes. Patients experienced fewer complications and quicker recoveries, reinforcing that home-based care can be both compassionate and cost-effective.
Cost Effectiveness Of The Presidium Model
Presidium Health’s model demonstrates that high-quality care doesn’t have to come at an exorbitant cost. By reimagining healthcare delivery, the organization significantly reduced unnecessary ER visits and hospital stays, which are often major contributors to healthcare spending.
For example:
- Reduced Healthcare Costs: The average annual cost for participants dropped from $17.9 million to $11.9 million.
- Better Resource Utilization: A lean approach helped cut redundant or unproductive spending across medical and logistical resources.
Dr. Afshar emphasizes, “Patients in value-based care models have better outcomes because the dollars go where they matter — directly to supportive, effective services.” This success showcases how innovative care delivery can stretch dollars further and simultaneously deliver exceptional care. For more insights into Presidium Health’s strategies, read Addressing SDOH in California.
Presidium Health’s value-based model isn’t just a blueprint for smarter spending; it’s a testament to how compassionate, patient-centric care can drive the future of healthcare.
Impact on Patient Health Outcomes
The HAH model isn’t just about cost savings or convenience—it profoundly improves patient health outcomes. By tailoring care to individual needs and delivering it in the comfort of patients’ homes, this model addresses the root causes of avoidable health complications. Results from these programs highlight a strong correlation between at-home care and measurable improvement in health metrics.
Reduction in Hospitalizations
A primary benefit of HAH initiatives lies in their ability to significantly cut hospitalization rates. Studies have consistently shown reduced inpatient admissions among participants. For example, one program cited a 38% reduction in hospital costs while also cutting down readmission rates to just 7% compared to 23% in traditional care models.
This reduction is driven by:
- Prompt access to 24/7 care teams.
- Implementation of remote monitoring tools that identify issues early.
- Focused care that minimizes unnecessary emergency room visits.
Further, Presidium Health’s pilot program achieved a remarkable 53% decrease in hospitalizations, showcasing the effectiveness of a risk-based, patient-centric approach. As Dr. Afshar, explains, “When care teams are proactive, and we meet patients where they are, the system itself becomes preventative.”
Patient Satisfaction and Engagement
Hospital-at-Home programs also transform the patient experience. Patients frequently report higher satisfaction levels, citing the comfort, personalization, and reduced stress compared to traditional hospital stays. Who wouldn’t feel more at ease receiving care in their own bedroom rather than a hospital ward?
Key factors driving satisfaction include:
- Personalized Care Plans: Care is tailored to meet specific health needs.
- Familiar Environments: Recovery at home promotes comfort and peace of mind.
- Reduced Infections: Avoidance of hospital-acquired infections leads to quicker recoveries.
Surveys often highlight how HAH programs improve patient engagement. Patients feel empowered to participate actively in their care processes. Dr. Afshar emphasizes, “Engagement is about communication—listening to patients and addressing their concerns in real time strengthens trust and enhances outcomes.”
A study by The Commonwealth Fund affirms these benefits, noting that participants regularly express higher satisfaction compared to those in inpatient settings. This renewed confidence fosters continuous care adherence, further improving long-term health outcomes.
By addressing both logistical and emotional barriers, Hospital-at-Home programs are rewriting the rules for patient-centric care. Wouldn’t every patient choose tailored, in-home care if it’s designed for better health outcomes and satisfaction?
Future of Hospital at Home Initiatives
As the healthcare industry continues evolving, the Hospital-at-Home model stands out as a pivotal transformation. This patient-centric approach has the potential to redefine acute care delivery while addressing rising healthcare costs. But what does the future of Hospital-at-Home look like? Below, we dissect the trends, legislative backing, and funding opportunities reshaping its growth trajectory.
Industry Trends
The Hospital-at-Home approach is gaining traction across multiple healthcare ecosystems. Industry trends underscore the shift toward at-home medical services in response to demand for scalability, efficiency, and patient satisfaction. Several key developments are shaping the course of HAH initiatives:
- Telemedicine Expansion: The normalization of telemedicine during the COVID-19 era enhanced public acceptance of remote healthcare. Technologies such as remote patient monitoring and virtual consultations are now cornerstones of HAH programs. For further insights into how telehealth drives innovations, visit The Role of Remote Technology in Healthcare.
- Care Personalization: Research indicates patients in HAH programs appreciate the individualized care plans tailored to their unique needs. This personalization is a growing trend that healthcare providers can no longer ignore.
- Integration with Value-Based Care Models: With value-based care models on the rise, HAH serves as a prime solution for cutting unnecessary costs while improving clinical outcomes.
Additionally, the technology supporting Hospital-at-Home care has grown exponentially. Tools like wearable devices now deliver real-time health data, enabling informed and prompt clinical decisions. This trend aligns with the findings in Providers Betting Big on Future of Hospital at Home, where the emphasis on cost savings and scalability is outlined.
Legislative Support and Funding
The future of HAH greatly depends on legislative policies and funding. Current frameworks show significant promise in fostering the growth of these programs.
- Medicare Waivers: The Centers for Medicare and Medicaid Services (CMS) introduced waivers during the pandemic to support acute care at home. These temporary policies paved the way for broader application. Policymakers are now reviewing options to make these waivers permanent, a move supported by industry leaders like Dr. Bruce Leff.
- Funding Initiatives: Large-scale funding ensures that the infrastructure supporting HAH programs flourishes. Institutions such as CMS have illustrated through various initiatives that sustained financial backing is crucial. Insights from The Acute Hospital Care At Home Waiver And The Future discuss the potential of funding to develop new service lines.
- Incentive Structures: Value-based care reimbursement models are likely to play a major role. These frameworks incentivize healthcare systems to innovate further, aligning with patient outcomes rather than patient volumes.
One concern, however, is navigating the initial investment cost for non-traditional hospital services. Healthcare executives must weigh the up-front financial commitment against long-term savings and improved patient outcomes. Leaders like Dr. Afshar underline, “A sustainable financial model and forward-thinking legislation are the twin engines driving the success of Hospital-at-Home.”
As the legislative landscape evolves, the role of funding and favorable policies will define the next phase for HAH programs. A closer look at academic studies, such as The hospital at home in the USA: current status and future, reveals optimistic adoption outlooks.
The future of Hospital-at-Home initiatives is undoubtedly exciting. With the healthcare industry leaning toward personalized, value-driven care, and legislative momentum supporting its expansion, this model could soon become a standard in global acute care delivery.
Conclusion
Hospital-at-Home reimagines the future of healthcare by delivering hospital-level care directly in patients’ homes. Its ability to reduce costs while improving outcomes positions it as a shift from traditional care models to more personalized solutions. As Dr. Pouya Afshar affirms, “This model represents an evolution toward quality-driven, value-based care.”
Integrating robust technology, committed healthcare teams, and patient-centered strategies, Hospital-at-Home accelerates recovery and elevates patient satisfaction. The success of such models underscores the necessity of innovation in tackling both logistical and health disparities. As the healthcare landscape adapts, this approach stands poised to play a crucial role in the era of advanced care delivery.
